Diabetic Foot Disease-How to Prevent and Treat it

Image Source: FreeImages
Table of Contents
Introduction
People with diabetes tend to have an increased risk of developing peripheral arterial disease (PAD) and its secondary complications, like ulcers and infections of the feet. The risk is further elevated if a patient has both diabetes and another chronic condition, such as peripheral neuropathy, nephropathy, or retinopathy.
In fact, diabetic foot disease is the most common complication associated with diabetes. It’s also one of the most challenging conditions for people with diabetes to manage because it has so many different subtypes.
Even more challenging is the fact that there are no universal measures that can be taken to reduce the risk of these complications— they are so strongly associated with type 2 diabetes specifically that nothing else really comes close. Therefore, this article will highlight everything you need to know about diabetic foot disease including its potential causes and how you can prevent or treat it if you develop it.
The statistics
Foot complications in diabetes are a leading cause of the global burden of disability.49 Global prevalence of foot complications include 131.0 million people (1.77% of the global population) with diabetes-related lower-extremity problems, incorporating 105.6 million (95% UI 85.5–128) with neuropathy only, 18.6 million (15.0–22.9) with foot ulcers, 4.3 million (3.7–4.9) with amputation without prosthesis, and 2.5 million (2.1–3.0) with amputation with prosthesis.50
Source- Sciencedirect.com
Long and short of it
If you prefer a quick take on what is written in this article, do try the slide show presentation below-
Types of Diabetic Foot Disease
Depending upon the cause, there are 5 different types of diabetic foot disease presentations: –
- Diabetes-related ulcers –
- This can lead to skin breakdown, which is the most common form of diabetic foot disease, particularly in the toes and the balls of the foot.
- Diseases of the bones and joints –
- Arthritis, osteoarthritis, and other diseases of the joints can be common in people with diabetes, especially those with peripheral arterial disease [PAD].
- This can present as pain, stiffness, and limited mobility. –
- Osteomyelitis
- This is an infection of the bone and bone marrow, usually caused by bacteria entering the bloodstream.
- It can spread to tissues and is thus also a risk for the muscles, nerves, and skin.
- Diseases of the arteries, veins, and lymph vessels –
- PAD, in which arteries are narrowed or blocked, is the most common cause of this.
- PAD can lead to vein clots and a potential pulmonary embolism, and veins can become inflamed and swollen, resulting in venous stasis ulcers (VSU).
- Diseases of the nerves –
- People with diabetes are also at higher risk of peripheral neuropathy, which can cause pain, numbness, and/or tingling in the lower extremities.
- Because of the loss of sensation, people with diabetes have decreased ability to feel pain associated with cuts, sores, and other injuries on the foot.
Potential Causes of Diabetic Foot Disease
There are numerous potential causes behind diabetic foot disease. The most common ones are: –
- Skin breakdown: Diabetic foot disease is often caused by skin breakdown, which can be caused by conditions such as pressure ulcers, corns and calluses, ingrown toenails, and blisters. –
- Arterial and venous diseases: PAD, hemangiomas, thrombosis, and other vascular diseases can cause pain and/or discomfort in the feet. –
- Neuropathies: Neuropathies can cause pain, numbness, and/or tingling in the feet that can often be misdiagnosed as diabetic foot disease when the cause is actually a compression nerve injury.
How to Prevent Diabetic Foot Disease

As the title suggests, the best way to prevent this debilitating and destructive disease is to prevent diabetes in the first place. If you have type 2 diabetes, the following steps can help prevent diabetic foot disease: –
- Stay informed and on top of your health: The best way to know if you have diabetic foot disease is to check your feet on a regular basis.
- Check your blood sugar regularly and see that it remains under the specified limit. The best way to do this is by using a good glucometer.
 Get it on Amazon in other countries- Canada, UK, India
Get it on Amazon in other countries- Canada, UK, India - Look out for callouses on the sole of the foot/feet. I would advise having a look at your foot sole by using a mirror to rule out formation of calluses/fresh wounds as diabetes can dull your sensation.
- Look out for any darkening of the skin- either black, blue or purplish.
- Avoid the temptation to scratch your foot if there is itching. Speak to your doctor about this.
- Avoid sprains/injuries to foot or ankle- that can lead to Charcot foot. You can visit a podiatrist or wear protective footwear as shown below.
- Try to feel the sensation on your feet-both from above and below. If you notice the lack of sensation, visit your doctor.
- Check the web of your toes and nails to rule out fungal infection.
- Wear diabetic footwear: Wearing appropriate footwear for your activity level, particularly for diabetes-related complications, will help reduce the risk of developing diabetic foot disease.
- You can read more about it here-” Diabetes and Your Feet“
How to Treat Diabetic Foot Disease
Treatment of Diabetic foot disease always starts with proper investigations as to the cause of this condition in the first place. First and foremost, rule out hyperglycemia, as to how much more the blood sugar and HbA1C is.
Then, check your Lipid profile to rule out high cholesterol levels- they can cause narrowing of peripheral arteries in your legs. Next, do a Color Doppler study of the leg or foot affected.
In some cases, an antibiotic culture sensitivity is carried to help prescribe appropriate antibiotics.
Depending on the outcomes of these investigations, a plan will be suggested by your treating physician. Treatment would be comprehensive taking into consideration the results of these investigations like proper control of your blood sugar, reducing your cholesterol levels, and prescribing the right antibiotic to control infection.
The Preliminary Treatment
If you have diabetic foot disease, it’s important to seek treatment as soon as possible. In some cases, it can be treated with lifestyle changes, but in others it may require surgical or medical intervention. Here is what you can do-
1.Bandaging and elevation:
In order to prevent further tissue damage and facilitate healing, you should bandage the wound and elevate the foot until it heals.
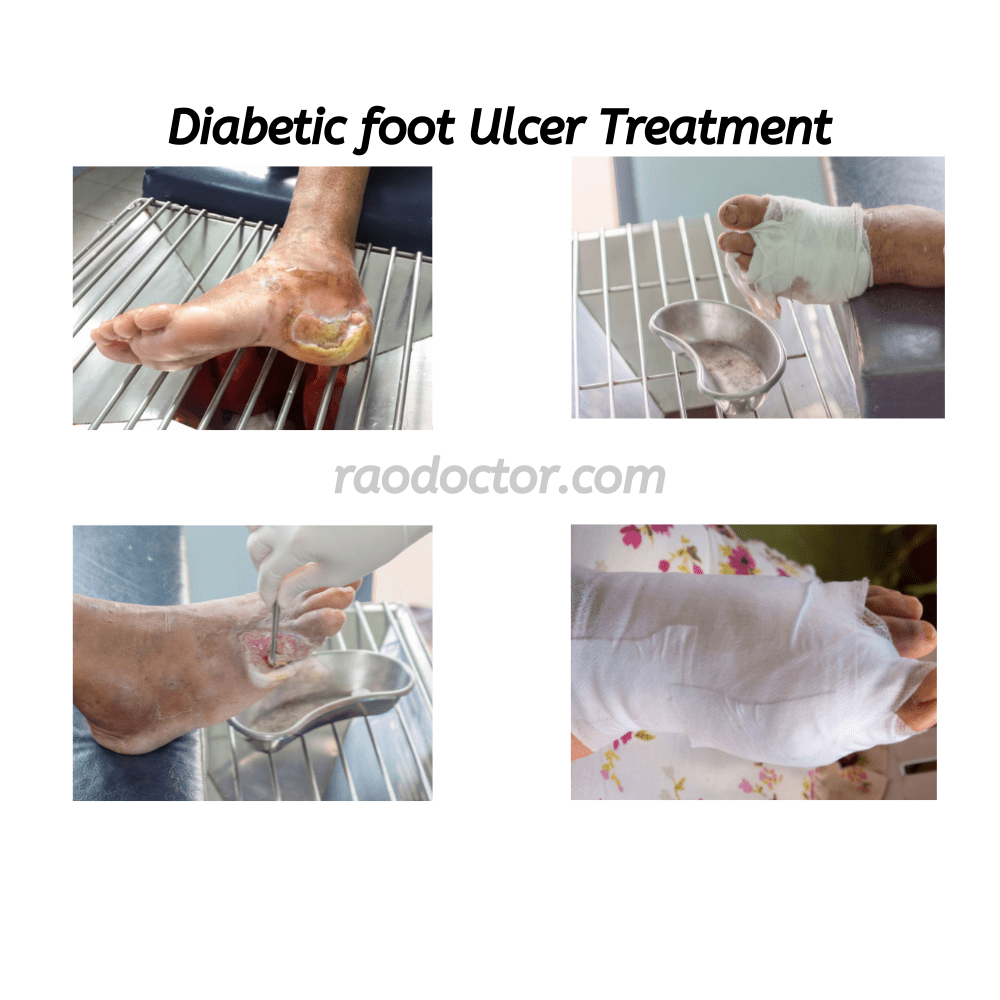
Step-by-step method of dressing a diabetic foot wound or ulcer-




2. Antibiotics and Anti-inflammatory drugs:
If there is an infection associated with diabetic foot disease, antibiotics should be administered as soon as possible to prevent the spread of the bacteria and the development of complications.
Depending upon the severity of the condition, your doctors might suggest strong antibiotics such as-
- Amoxycillin and clavulanic combinations- e.g., Augmentin Duo, Erox 625.
- Cefixime and clavulanic acid combinations- e.g., Zifi CV 200.
- Cefixime and ofloxacin combination- e.g. Zifi-O.
Anti-inflammatory drugs like combinations of diclofenac- serratiopeptidase [ e.g., Emanzen-D] or diclofenac- Trypsin-chymotrypsin-rutoside combination[ Enzoheal-D] help a lot in reducing inflammation.
You can get these medicines by uploading a prescription on-
3. Restoration of blood supply:
In the case of an arterial occlusion (thrombosis), blood flow should be restored to reduce the risk of tissue death and amputation.
If the arteries of the legs have been blocked totally, your doctor may suggest you go a vascular surgeon who will restore the blood supply by either-
- Bypass graft or
- By putting a stent in the affected artery.
4. Neuropathy:
High blood sugar levels also affect the nerves that supply the foot causing loss of sensation thereby causing unnoticed injuries and ulcer formation.
Peripheral Neuropathy is one of the diseases of the nerves that can cause diabetic foot disease, and it’s treated with-
- Tight blood sugar control,
- Nutritional supplements containing high dose of Vitamin B12 and gabapentin, e.g., Meganeuron PG, Pregaba NT.
Conclusion
This article has highlighted everything you need to know about diabetic foot disease. It’s important to understand the potential causes and symptoms of diabetic foot disease so that you can recognize the condition as soon as it develops. If you are diabetic, it’s important to be aware of your risk of developing diabetic foot disease and take the necessary steps to prevent it.
With the right knowledge, foot care, and treatment, diabetic foot disease can be managed successfully.DIABETIC FOOT DISEASE-5 Suggestions on HOW TO PREVENT OR TREAT IT Share on XDisclosure-
This article contains links to Amazon.com and Canva Pro, that if clicked and a purchase made using the link. can help the author earn a small commission without any extra charge to the purchaser. This can help maintain this website and get you useful articles absolutely free every time a new article is published.