Table of Contents
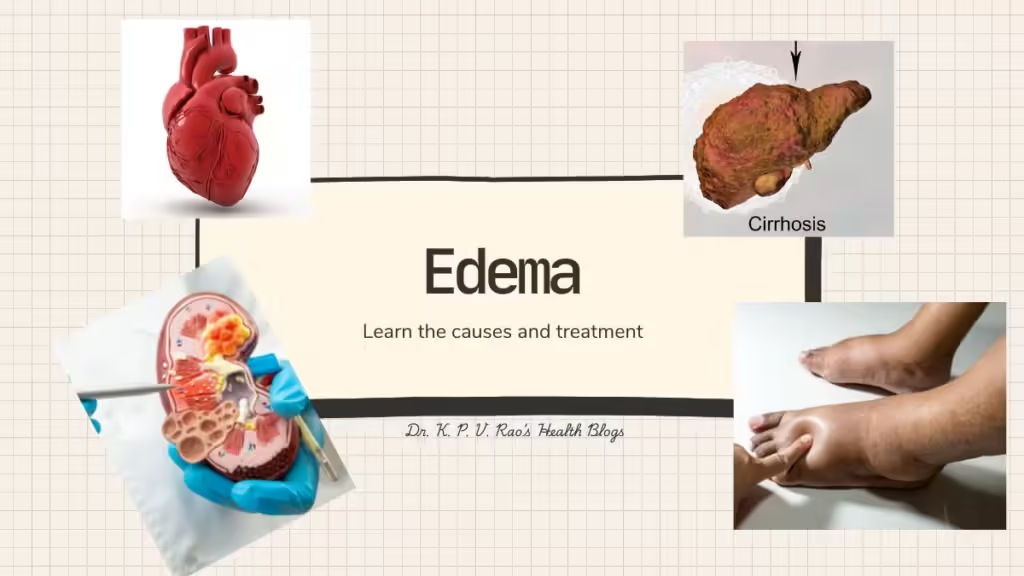
What is Edema?
Edema refers to the medical condition characterized by the accumulation of excess fluid within the body’s tissues, leading to noticeable swelling of body part or parts affected.
This swelling most frequently affects the extremities, such as the legs, feet, and ankles, but it can also occur in other areas, including the face and hands.
Edema can range from mild and transient to severe and persistent, often hinting at underlying health issues or lifestyle choices.
Understanding the physiology behind fluid balance is crucial to grasping how disruptions can lead to edema.
How does edema occur?
The human body maintains fluid balance through a series of intricate processes involving the circulatory, lymphatic, and renal systems. Blood vessels, specifically capillaries, work in conjunction with the lymphatic system to ensure that fluids are distributed and reabsorbed appropriately.
When these systems function correctly, fluid stays within the blood vessels and interstitial spaces—the small gaps between cells—maintaining a stable environment.
However, when abnormalities arise in these physiological processes, fluid may leak into the interstitial spaces, resulting in edema.
What types of edemas do we come across?
The causes of edema are varied and can be classified broadly into two types: localized and generalized. Localized edema is confined to a specific region, such as the swelling that occurs in an injured or sprained ankle.
Generalized edema, on the other hand, involves the accumulation of fluid throughout the body and is often a sign of systemic illnesses like heart failure, kidney disorders, and severe malnutrition. Recognizing the distinctions between these types is essential for diagnosis and treatment.
What are the factors leading to formation of edema?
Several factors can contribute to fluid imbalances, leading to edema. We have some medical conditions and some lifestyle habits. Let’s what they are-
Medical conditions such as:
- congestive heart failure,
- liver disease such as cirrhosis, and
- Kidney dysfunction is a notable cause.
Lifestyle habits such as:
- prolonged sitting or standing,
- excessive salt intake, and
- certain medications, including steroids and antihypertensives, can also result in fluid retention.
Understanding the underlying reasons for edema is key to implementing effective management and therapeutic interventions.
In essence, edema serves as a warning signal that something may be amiss within the body’s fluid regulatory systems. Identifying the type and cause of edema allows for targeted approaches to treatment, aiming to restore fluid balance and reduce swelling.
Causes of Edema
Fluid retention in various tissues, characterized by the swelling of tissues due to excess fluid retention, can result from numerous factors.
As said above, one of the most common causes is the prolonged duration of standing or sitting, as these positions can impair the effective circulation of blood, leading to fluid accumulation in the lower extremities.
Another significant contributor is the excessive intake of salt, which disrupts the body’s sodium-water balance, prompting the retention of additional fluid to dilute the high sodium levels.
Several medical conditions also play a crucial role in the onset of edema. Heart disease is a prime example, where the heart’s reduced efficiency in pumping blood leads to fluid build-up in various body parts, most notably the legs and feet.
Likewise, liver disease, particularly conditions such as cirrhosis, can impair the organ’s ability to produce proteins that help maintain fluid balance. As a result, fluid leaks into the surrounding tissues, causing swelling.
Kidney disease, on the other hand, affects the body’s ability to expel excess fluids and sodium, leading to widespread edema.
Development of edema-the mechanism
The vascular and lymphatic systems are integral to understanding the development of edema. The vascular system, which includes veins and capillaries, is responsible for the effective return of blood to the heart.
Any condition that impacts this system, such as chronic venous insufficiency, can result in fluid leakage into tissues.
Similarly, the lymphatic system, which drains excess fluids from the tissues, when compromised due to conditions like lymphedema [as in filiarasis or elephant foot], results in significant swelling.
Moreover, pregnancy and hormonal changes can induce temporary edema. The hormonal fluctuations during pregnancy cause the body to retain more water, while the growing uterus can exert pressure on the veins, impeding blood flow and causing swelling in the lower body’s tissues.
Useful Reference: Mayo Clinic-Edema
Diseases and Conditions That Cause Edema
Unusual accumulation of fluid in the tissues can manifest due to several underlying diseases and conditions. Understanding the etiological agents behind this symptom is crucial for both diagnosis and treatment.
Among the most prevalent conditions that precipitate edema is congestive heart failure (CHF). In CHF, the heart’s diminished pumping efficiency leads to an increase in pressure within the blood vessels. This pressure pushes fluid from the blood vessels into the surrounding tissues, causing swelling.
Another condition that significantly contributes to the development of this acculamation of fluids is cirrhosis of the liver. In cirrhosis, the liver’s normal architecture is replaced with fibrosis and regenerative nodules. This leads to a disruption in the production of albumin, a protein essential for maintaining oncotic pressure. A decline in oncotic pressure means that fluid tends to leak out of blood vessels into the surrounding tissues, manifesting as edema.
Kidney disorders, especially nephrotic syndrome, are also notable contributors to the onset of edema. In nephrotic syndrome, there is significant protein loss in the urine, which reduces oncotic pressure similarly to cirrhosis. The kidneys also lose their ability to regulate sodium and water balance, exacerbating fluid retention and contributing further to swelling.
Chronic venous insufficiency (CVI) offers another pathway through which acculamalation of fluids occurs in the legs. In CVI, the veins in the legs are unable to pump blood back to the heart efficiently, often due to damage or secretion inadequacies in the valves. This inefficiency leads to a pooling of blood in the lower extremities. The accumulated pressure from pooled blood drives fluid out of the veins and into the tissues, resulting in swelling.
Each of these conditions interferes with the body’s normal mechanisms for fluid regulation, whether through alterations in oncotic pressure, impaired organ function, or disrupted vascular integrity. Understanding how these diseases cause fluid imbalance provides a framework for managing and treating edema more effectively.
Medications and Lifestyle Treatments
Treating edema effectively requires a multifaceted approach that often combines pharmacological treatments with lifestyle modifications. The primary goal is to address the root cause of the fluid retention and provide symptom relief.
Diuretics, commonly referred to as water pills, are frequently prescribed to help the body eliminate excess fluid. These medications work by increasing urine production, thereby reducing fluid buildup in tissues. However, while diuretics can be effective, they must be used under careful medical supervision to avoid potential side effects such as electrolyte imbalances.
Apart from pharmacological interventions, various non-drug strategies are essential in managing edema. Dietary adjustments play a critical role; for instance, limiting salt intake can significantly reduce fluid retention.
Sodium in salt can cause the body to retain water, so cutting back on salty foods is a practical step towards reducing swelling. Staying well-hydrated by drinking appropriate amounts of water is also vital, as dehydration can paradoxically promote fluid retention.
Physical strategies like elevation and the use of compression stockings can offer considerable relief. Elevating the affected limbs helps facilitate the drainage of excess fluid back towards the heart, reducing swelling.
Compression stockings support circulation by applying gentle pressure to the legs, preventing fluid from pooling in the lower extremities. Consistent physical activity, such as walking or swimming, enhances blood circulation and helps move fluid through the lymphatic system, reducing fluid retention in the legs.
In more severe cases of edema, medical interventions may be necessary. These can include procedures to remove fluid manually, such as paracentesis or thoracentesis, particularly in cases of severe fluid accumulation in the abdomen or chest.
Conclusion
For individuals whose edema is linked to chronic conditions like heart failure or kidney disease, managing these underlying conditions is paramount to controlling swelling.
Overall, the management of fluid accumalation requires a comprehensive approach that combines both medication and lifestyle changes. By addressing the underlying causes and employing various strategies, effective relief from edema can be achieved.
Final words
I hope I have been able to explain the concept of unhealthy body swelling due to fluid accumalation in various tissues of our body.