Table of Contents
Part 1- What is retinal detachment and what are its consequences
Welcome to a comprehensive guide on understanding retinal detachment! In this article, we will explore the causes, symptoms, and treatment options related to this serious eye condition.
Recently, I wrote an article on 4 age-related Eye disorders. Out of them, one was retinopathy- disorder of the innermost layer of the eye- yes, you guessed it rightly- the retina.
Of late, I have observed patients visiting my clinic with a variety of visual symptoms. Some have blurred vision, some say they see some bubbles floating in front of their eyes while reading, while some have come with complaints of loss of sideways vision or complete loss of vision in one eye.
These patients are then referred to an ophthalmologist for further evaluation and treatment. The frequency of post cataract operation complications is on the rise and the most common amongst them are those with retinal detachment, macular edema and age-related macular degeneration. We will be dealing with the topic of retinal detachment in this article.
One of my learned patients, who visited me recently, has this to say-
Life is full of uncertainty. Expect the unexpected and get seasoned with the unexpected.
A learned patient
The same thing is true of retinal detachment- an eye condition which happens unexpectedly in some people.
Here are some examples of this happening in two of my patients:
Case study no. 1
A 70-year-old patient suddenly started seeing floaters in one of his eyes post cataract operations that was performed 2 years back. A part of his eye was not able to perceive any sight. He was referred to an ophthalmologist who, after a thorough eye check-up declared that he had retinal detachment. He has been undergoing treatment for Hypertension for the past 10 years.
Case study no. 2
Another 70-year-old patient, Mr. JRM, who was a diabetic, started getting blurred vision after 3 years of cataract surgery. He was also referred to an ophthalmologist who told him that he had retinopathy and retinal detachment.
Now, even though the eye problems of both these cases had the same ailments, they both have different causes and treatment background.
We will come to the management of these two cases in Part 2 of this article.
So, what exactly happens in Retinal Detachment?
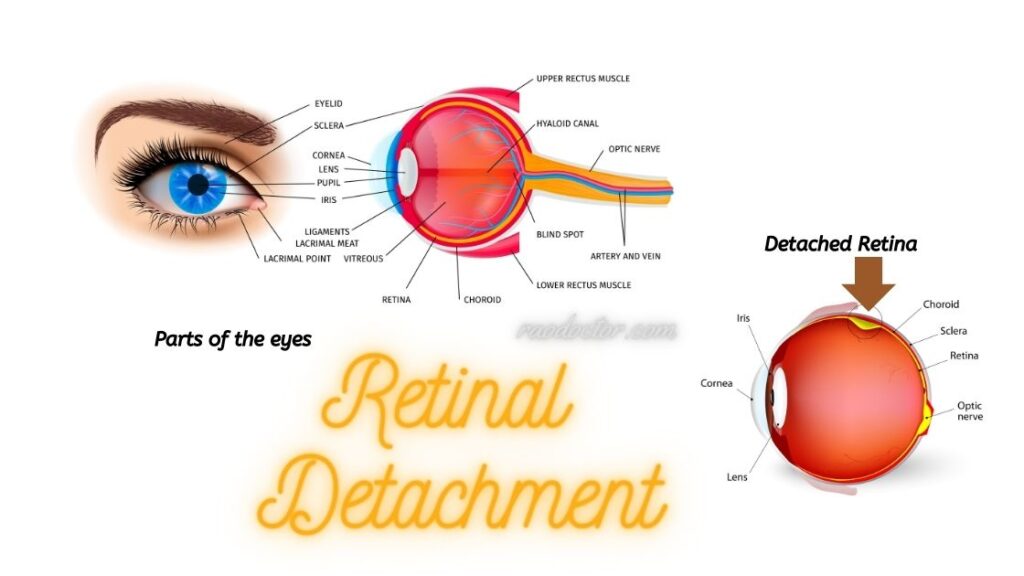
Retinal detachment [RD] occurs when the thin layer of tissue at the back of the eye called Retina [have a look at the image below], responsible for capturing light and sending visual signals to the brain, detaches from its normal position.
It is crucial to be knowledgeable about this condition, as early detection and prompt treatment can potentially preserve your vision.
In the past I had given information on Diabetic Retinopathy– you can read it here if you have not read it yet-
We will delve into the different factors that can lead to retinal detachment, including trauma, age-related degeneration, and underlying health conditions. As this article is quite exhaustive, I have decided to split this article into 2 parts.
In Part 1, we will highlight the common symptoms to watch out for, such as sudden flashes of light, a sudden increase in floaters, and a curtain-like shadow in your peripheral vision. We will also learn about the causes of retinal detachment.
In Part 2, we will explore the methods to diagnose and available treatment options, ranging from laser surgery and cryotherapy to vitrectomy along with ideas to prevent retinal detachment.
So, let’s get started on this informative journey to better understand retinal detachment and take proactive steps towards preserving your precious sight.
Anatomy and Function of the Retina
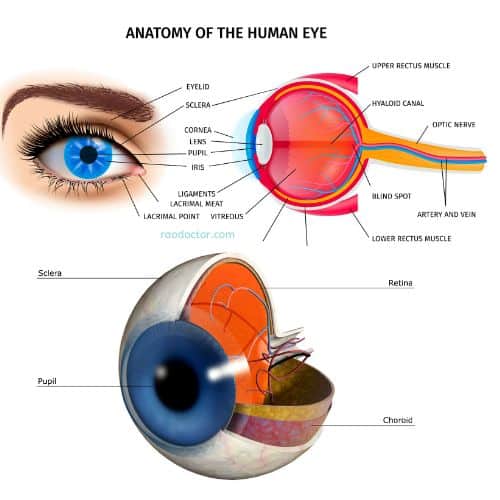
To grasp the concept of retinal detachment, it is essential to understand the anatomy and function of the retina. The retina is a thin layer of tissue located at the back of the eye, as you can see in the picture above.
Its primary role is to capture light and convert it into neural signals that are then transmitted to the brain through the optic nerve.
This intricate process allows us to perceive and interpret visual information. The retina consists of several layers, including the photoreceptor layer, which contains specialized cells called rods and cones that are responsible for detecting light.
These cells convert light into electrical impulses, which are then transmitted to the brain through the optic nerve for further processing. These electrical impulses are then recognized by the brain as images that we see.
The retina is supported by a gel-like substance called the vitreous, which fills the space between the lens and the retina. This gel provides essential nutrients to the retina and helps maintain its shape and position.
However, in some cases, the vitreous can pull away from the retina, leading to a condition known as posterior vitreous detachment (PVD). While PVD itself does not typically cause retinal detachment, it can increase the risk of detachment occurring in susceptible individuals.
Causes of Retinal Detachment
Retinal detachment happens when the retina becomes separated from its normal position. This detachment disrupts the flow of nutrients and oxygen to the retina, potentially leading to permanent vision loss if not addressed promptly.

Understanding the causes of retinal detachment is crucial in identifying risk factors and seeking appropriate treatment.
Retinal detachment can occur due to various factors, both traumatic and non-traumatic.
Traumatic causes include:
- direct injury to the eye, such as a blunt force impact or
- penetrating injury.
These types of injuries can cause the retina to tear or detach due to the sudden force exerted on the delicate tissue.
Non-traumatic causes are often related to age-related changes in the eye or underlying health conditions.
Age-related degeneration is one of the primary causes of retinal detachment. As we age, the vitreous gel inside the eye can become more liquefied and shrink, leading to posterior vitreous detachment [PVD]. When the vitreous detaches from the retina, it can sometimes cause small tears or holes in the retinal tissue. These tears can then allow fluid to accumulate between the retina and the underlying layers, leading to detachment.
In addition to age-related changes, certain underlying health conditions can increase the risk of retinal detachment. For example, individuals with severe nearsightedness (myopia) are more susceptible to retinal detachment due to the elongation of the eyeball, which can put additional strain on the retina. Other conditions, such as diabetic retinopathy, can also contribute to retinal detachment by weakening the blood vessels that supply the retina with essential nutrients.
Risk Factors for Retinal Detachment
While anyone can potentially develop retinal detachment, certain factors can increase the risk. Here are the commonly known risk factors:
Age
is a significant risk factor, as the incidence of retinal detachment tends to increase with age. Individuals over the age of 40 are more prone to this condition, particularly if they have other underlying risk factors.
Severe nearsightedness, or myopia,
is another significant risk factor. The elongation of the eyeball in myopic individuals can put additional strain on the retina, making it more susceptible to tears or detachment. If you fall into this category, it’s essential to be vigilant about any changes in your vision and seek regular eye examinations to monitor your eye health.
Previous eye surgeries or injuries
can also increase the risk of retinal detachment. If you have undergone cataract surgery or have experienced an eye injury in the past, it is crucial to inform your eye care professional about your medical history. They can provide appropriate guidance and monitor your eyes for any signs of retinal detachment.
Other risk factors
This includes:
- a family history of retinal detachment,
- certain genetic disorders, and
- certain systemic conditions like diabetes.
If you have any of these risk factors, it’s important to be proactive in monitoring your eye health and seeking regular eye examinations to catch retinal detachment early, if it were to occur. Early detection and timely intervention by your ophthalmologist may help save eyesight or further damage to retina.
Symptoms of Retinal Detachment
Recognizing the symptoms of retinal detachment is vital for early detection and prompt treatment. While some cases of retinal detachment may be asymptomatic, there are several common signs that should not be ignored. If you experience any of the following symptoms, it is crucial to seek immediate medical attention to determine the cause and receive appropriate treatment.
- One of the most noticeable symptoms of retinal detachment is the sudden onset of flashes of light in your vision.
- These flashes may appear as brief, bright streaks or flickering lights at the periphery of your visual field.
- They can occur sporadically or persistently, and their presence should never be disregarded.
- Another symptom to watch out for is the sudden increase in floaters. Floaters are tiny specks or cobweb-like structures that float across your field of vision.
- While they are usually harmless and a normal part of the aging process, a sudden increase in the number or size of floaters can be a warning sign of retinal detachment.
- If you notice a sudden shower of floaters or the appearance of a significant floater that obstructs your vision, it is crucial to seek immediate medical attention.
- A curtain-like shadow or veil descending across your visual field is another symptom that may indicate retinal detachment.
- This shadow is typically peripheral and may progress towards the center of your vision if left untreated.
- If you experience the sensation of a curtain or a dark shadow obstructing your sight, it is imperative to consult an eye care professional as soon as possible.
It’s important to note that these symptoms can also be caused by other eye conditions, such as vitreous floaters or migraines. However, since retinal detachment is a serious condition that requires immediate medical attention, it is always better to err on the side of caution and seek professional evaluation.
Dr. K. P. V. Rao’s Health Blogs
We now come to the end of Part One of this article. I hope you have fully understood the seriousness of retinal detachment.
To be continued……..
In my next article we will learn all about investigations, diagnosis and management of retinal detachment.
If you have found this article useful, please promote it by sharing on social media by clicking on the icons at the bottom of this article. Alternately, you can Click to Tweet here-
Understanding Retinal Detachment: Causes, Symptoms, and Treatment Options Share on XAdios.