Diabetic Retinopathy-How to avoid it and have a better vision
 What is Diabetic Retinopathy?
What is Diabetic Retinopathy?
In simple words, Diabetic Retinopathy refers to the eye complication of diabetes caused due to poor blood sugar control. It is the major cause of blindness in advanced Type 2 and in Type 1 diabetes. It is also called the “blurry vision of diabetes type 2”.
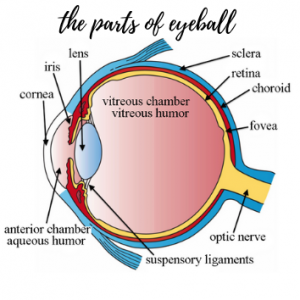
Before we proceed ahead with how one gets to this condition, let’s make ourselves familiar with the structure of the eyeball.
Anatomy of the Eyeball-
Have a good look at this picture of the eyeball-
The reason behind showing this anatomical picture of the eye is that almost all structures shown can get affected by a high blood glucose level in Diabetes. The collective conditions of eye diseases in diabetes are termed Ocular Eye diseases. Now have a look at the same picture showing the affected parts of the eye- it reveals[in red color] some of the commonly encountered Ocular diseases-
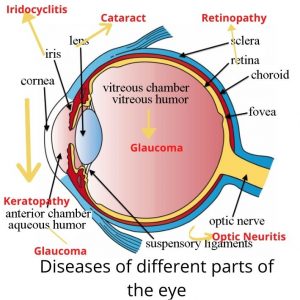
The disease affecting the screen of the eye- the Retina- is called Retinopathy and in the diabetic patient, it occurs early.
According to the authors of the book A Practical Guide to Diabetes Mellitus[shown below], “diabetic patients are 25 times more likely to suffer blindness other than nondiabetic patients matched for age and gender”.
To know more about the eye problems, I have designed a table showing different Ocular diseases[ as shown in the picture above] that occur in general and diabetes in particular.
Table of Ocular Diseases-

Out of all the Ocular Diseases, retinopathy of diabetes stands out as quite important because it is the major cause of various visual impairments, including blindness.
Why am I writing this article on Diabetic Retinopathy[DR]?
All the above conditions shown in the table above occur in diabetes. All the parts of the eyeball are necessary for having a good vision. Whereas some of the conditions such as refractory changes are correctable with the use of spectacles, and some with medications, retinopathy requires special attention.
According to a survey in October 2019, Diabetic retinopathy affected almost 16% of diabetics annually in India. It affects about 80% of those having Diabetes. Moreover, the longer a person suffers from diabetes, the more his/her chances of developing DR.
According to the Survey-
- About one in 46 diabetic patients in India become visually impaired due to diabetes.
- Retinopathy of diabetes was prevalent in the diabetic population for up to 50 years.
- 16.9% suffered from DR. Out of these, 17% were males and 16.7%, females
- Age-wise, retinopathy of diabetes was present as follows-
- 60-69 years-18.6%
- 70-79 years-18.3%
- 80 years and above-18.4%
The incidence of blindness among all diabetic patients was found to be 2.1% and visual impairment, 13.7%. This shows that out of 100 people suffering from diabetes, about 2.1% will suffer from blindness and about 13.7% will have some eyesight problems like blurred vision, double vision, cataract, etc.
These findings prompted me to write this article as our eye is one such organ that is very delicate and its disease will cost one dearly.
What are the risk factors for getting Retinopathy of Diabetes?
Diabetic retinopathy, as the name suggests, is due to poor control of blood sugar. However, this is enhanced by-
- High blood pressure or hypertension
- High Cholesterol levels\
- Smoking
- Alcoholism
All these conditions have a profound effect on the blood supply of the retina. They are known to narrow/block the arteries supplying the retina.
Case Study-
In my clinical practice also, I have come across a few cases with Diabetic Retinopathy. Here is one such example of findings in a case of diabetic retinopathy. About 20 years back, Mr. AM[real name hidden for privacy sake], was suffering from Type 2 diabetes and hypertension.
He was an alcoholic and did not bother about his health. One day he calls me up from his native place-New Delhi. He complained of a total loss of vision in the right eye and partially in the left eye. I enquired about his blood sugar[BS] level.
It was as follows –
- Fasting BS-250mg/dl
- Post-prandial[after meals]- 450mg/dl.
- HbA1c- above 11
I then suggested him to see an eye specialist[ophthalmologist] in Delhi and send me his reports and treatment suggested. By evening he reported the following findings-
- The right eye showed the detachment of retina because of which he had lost his vision. There was no hope of saving vision in this eye.
- The left eye showed inflammation of the retina with leakage of blood in the eye. He was going in for a condition called Diabetic Macular Edema[DME]. This was the cause of partial loss and blurring of vision in that eye.
I suggested that he come back to Mumbai which he did. After reviewing his case, I suggested the total abstinence of alcohol. With proper treatment, his blood sugar was brought under control.
Later, he was referred to a prominent retina surgeon in Mumbai. The Surgeon managed to salvage most parts of his left eye retina and saved him from total blindness.
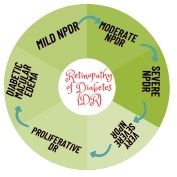
Are there any Stages of Diabetic Retinopathy?
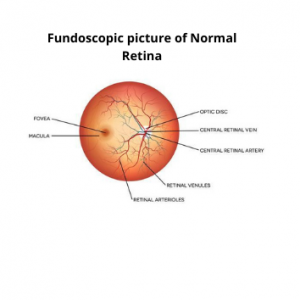
Let us first study how the Retina looks like and what are its parts. If the retina is normal, this picture will be seen by your eye specialist when you visit him to rule out DR. Have a look at this picture-
Picture 1-

All the different parts of the retina- the optic disc, the fovea, the macula, the blood vessels[the central retinal artery, retinal venules, retinal arterioles, central retinal vein] supplying the retina, etc., can get affected due to rising blood sugar levels.
Now, look at the picture below showing the changes in the retina of the eye as seen in the fundoscopy examination by your eye specialist-
Picture 2-

All these changes seen in retinopathy do not occur at the same time. There are various stages[discussed below] of retinopathy. The changes shown above occur gradually depending upon your blood sugar levels.
Uncontrolled diabetes or poor management of blood sugar levels causes changes in almost all parts of the eyes. These changes are slow to appear and the patient does not realize it initially. As shown in the picture above, changes start in the blood vessels of the eyes defining the different stages of Diabetic Retinopathy. Your ophthalmologist may suggest that you may have either of these stages-
- Mild Non-proliferative Retinopathy[NPDR]
- Moderate Non-proliferative Retinopathy
- Severe Non-proliferative Retinopathy
- Very Severe Non-proliferative Retinopathy
- Proliferative Diabetic Retinopathy
- Diabetic Macular Edema[DME]
This slideshow will take you quickly through the different stages changes we see in the Retinopathy of Diabetes –
What happens in Retinopathy of Diabetes?
Let us first consider the function of the retina. The retina is a thin lining at the back of the eye. It contains blood vessels[arteries and veins] and nerves. These nerves contain light-sensitive tissues that-
- Detects light.
- And interprets this light into electrical impulses.
- These electrical impulses are then transmitted to the brain through the optic nerve [see the anatomy of eyeball shown above] to form an image or picture.
The high blood sugar in diabetes causes changes in the retina-
- By damaging the tiny blood vessels supplying the retina-
- Leading to leakage of blood and fluid in the retina-
- Causing distortion of the image formed on the retina and this leads to a condition called Diabetic Retinopathy.
To know what happens in DR, let us go thru the sign, symptoms, and implication of the different stages mentioned above-
1.Mild Non-proliferative DR- 
This is the earliest stage of DR wherein there is a ballooning effect on the blood vessels of the retina. It is termed an aneurysm or more correctly-microaneurysm[ as seen in Picture 2]. Fluid like blood and plasma then leak through these microaneurysms and cause blurring of vision.
Sometimes these changes in the retina will not be felt by the patient. A proper blood sugar control at this stage will help in slowing the progress of the retinopathy to its next stage. And possibly reverse the eyesight to its original state.
2. Moderate Non-proliferative DR- 
If the patient has not felt the changes of the first stage, and his blood sugar control still remains to be poor, the retinopathy progresses to the second stage.
At this stage, there is swelling and distortion of the blood vessels which nourish the retina. There is leakage of blood products or blot hemorrhages in the retina.
These are termed soft exudates[cotton wool spots]. If you divide the retina into 4 quadrants, these cotton wool spots will be visible in at least in one of the quadrants.
There are changes in the veins also making them appear as a string of beads. This is called Venous beading.
3. Severe NPDR-
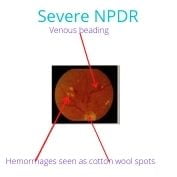
This stage is characterized by-
- Almost all the blood vessels of the retina get blocked leading to a lack of blood supply.
- Growth of newer blood vessels which we call collaterals. This happens due to the release of a growth factor called Vascular Endothelial Growth Factor[VEGF].
In this stage, you will see all the changes seen in Mild and Moderate NPDR along with-
- Microaeurysms or hemorrhages in all 4 quadrants of the retina.
- Venous beading in more than 2 quadrants
- All other symptoms of Stage 1 and Stage 2 DR
There is an increasing incidence of blindness. More than one part of the eye may get affected leading to loss of eyesight.
4. Very Severe NPDR-
This stage comprises of all the features of the above 3 stages plus –
- Increase in hemorrhages in all quadrants of the retina.
- New arteries and veins are formed that spread and cover most parts of the retina causing distortion of images formed on the retina.
- Swelling of the central most part of the retina- the Macula, causing more blurring of vision.
5. Proliferative DR-
This stage is characterized by an abnormal growth of blood vessels in the part of the retina called the optic disc[see Picture 1-Parts of Retina].
This is called the Proliferation of the vessels which spread and cover most parts of the retina.
This stage is common in Type 1 Diabetes and Type 2 patients on insulin.
If these new vessels grow into the Vitreous Chamber[ a jelly-like fluid in the eye-see Parts of Eyeball], they can-
- Cause an increase in eyeball pressure which results in Glaucoma leading to a sudden decrease in vision preceded by red floaters. Glaucoma can be detected by checking eyeball pressure by an instrument called tonometer.
- The detachment of the retina due to traction.
- Hemorrhage into the Vitreous chamber leading to pain in the eyes and a sudden decrease in vision.
6.Macular Edema-
This leads to changes in the Macula – the main part of the retina through which the blood vessels and nerves enter and leave the retina. These collective changes in the retina are termed Diabetic Macular Edema or DME.
What are the symptoms at this stage?
The eye vision starts deteriorating. The symptoms observed are-
- Blurred vision;
- Impairment of color vision-the patient may not be able to distinguish different colors.
- On and off of vision i.e. fluctuating vision. There can be blacking out of vision.
- Floaters in the vision i.e different shapes floating in front of the eyes while watching something. These appear as dark spots in the field of vision.
What are the symptoms to watch out for?
What we have discussed above are the signs that will be seen by your ophthalmologist. Most of the symptoms I have covered while discussing the stages of retinopathy.
However, if a diabetic patient is going in for retinopathy, he/she should look out for-
- Diminishing of vision
- Sudden-onset floaters: Black or red, moving on the movement of eyes, worse after waking up from sleep
- Painful red eye.
For easier and better understanding of Diabetic Retinopathy, read this article by Mayo Clinic.
Let us now move on to the treatment of these stages of retinopathy.
Treatment of Diabetic Retinopathy-
Let us divide this into 2 parts–
1.By your family physician-
It is your doctor’s responsibility to control your diabetes by-
- Suggesting appropriate medicines;
- Investigating regularly, particularly HbA1C and cholesterol levels;
- By advising a change of habits like smoking and alcohol consumption;
- Random blood sugar checks while you visit his/her clinic
2. By your ophthalmologist-
A detailed discussion of this is beyond the scope of this article as these procedures are difficult to understand. However, I will touch briefly upon some of the main components of what your eye surgeon may advise.
Depending on the stage of retinopathy, your ophthalmologist may suggest-
- Laser photocoagulation-to stop leaking microaneurysms and spread of diffuse retinal thickening.
- Subthreshold micropulse diode laser-to prevent retinal damage.
- Intravitreal anti-VEGF agents-to prevent macular edema.
- Pars plana vitrectomy-again to prevent macular edema and retinal detachment.
Let us now move on to something which we can really do-prevention of Diabetic Retinopathy.
How to prevent retinopathy or reduce risk of retinopathy-
If a diabetic patient sincerely follows these steps, there is a good chance of not getting Retinopathy of Diabetes-
- Check your blood sugar and HbA1C regularly
- Do not skip any medicines prescribed by your doctor. If there is any problem, discuss it with your doctor.
- Make lifestyle changes-control your weight and cholesterol levels
- Avoid smoking and alcohol
- If you notice any changes in your vision, promptly discuss it with your family physician and your ophthalmologist.
Conclusion-
As I come to the end of this blog/article, I would like to add that the Diabetic Retinopathy is such a condition that is very much preventable. Just follow the advice I have suggested above. If any of your loved ones are suffering from diabetes, you can help them from getting blind by reading out this article to them.
Finally, you should also read some more articles which I am suggesting below-
Read here to know more, click here-FYidoctors.com
And here-retinarisk.com
And here-msdmanuals.com
And here- harvard health publications
And here- Diabetic retinopathy
Finally, I strongly recommend that you should visit this site for getting proper and more guidance for Diabetes Care-
A word of gratitude:-
Friends, the knowledge that I have just shared with you is a collective effort by me to put the best available information available in books and the internet, albeit in a very simple format. The book ” A Practical Guide to Diabetes Mellitus” by the authors N Thomas, N Kapoor, J Velavan, and KS Vasan has been of great help in the writing of this article. I offer my sincere thanks to these authors.