Understanding Diabetic Neuropathy
Diabetic neuropathy is a nerve disorder caused by long-term uncontrolled diabetes, resulting in symptoms like numbness, tingling, and pain in the hands and feet. It occurs when high blood sugar levels damage the nerves over time.

This condition can significantly impact quality of life and pose serious health risks if left untreated. Understanding the causes and risk factors of diabetic neuropathy is crucial in managing the condition effectively.
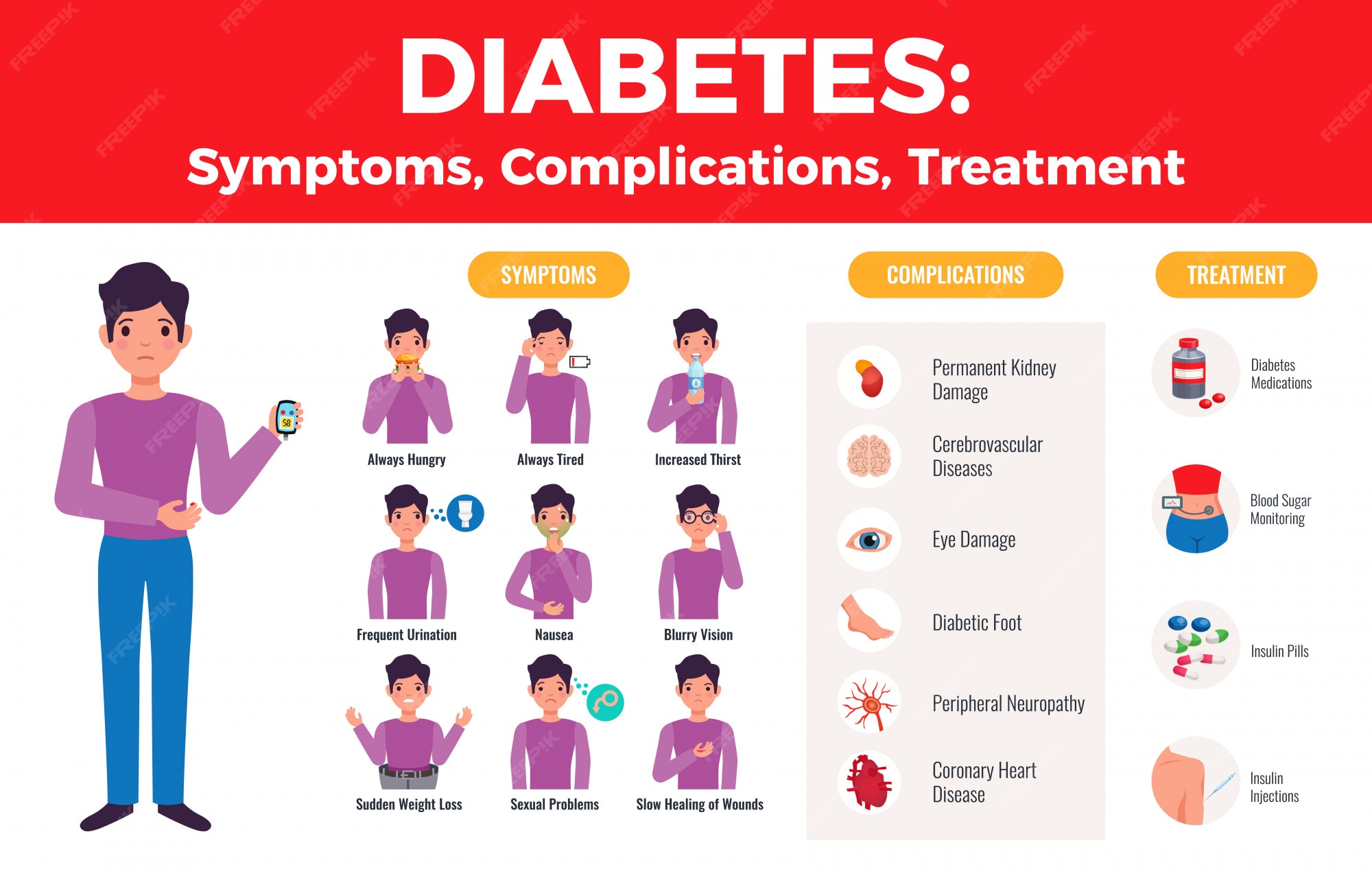
Have a look at the image infographic below- it tells you in short all about diabetes and its complications.
Living with diabetic neuropathy can be challenging, but there’s good news on the horizon. In this article, we’ll explore the latest breakthroughs and medicines that are revolutionizing the management of this condition.
Causes and Risk Factors of Diabetic Neuropathy
There are many complications of uncontrolled diabetes; my recent article was on Diabetic Kidney Disease and earlier I had published articles on diabetes affecting eyes and foot. Here is the link to all these articles if you have not read it yet-
The primary cause of diabetic neuropathy is prolonged exposure to high blood sugar levels. When blood sugar levels are consistently elevated, it can lead to nerve damage.
Mayo Clinic
Other factors that contribute to the development of diabetic neuropathy include :
- obesity,
- smoking,
- high blood pressure, and
- a sedentary lifestyle.
It is essential for individuals with diabetes to manage their blood sugar levels and address these risk factors to prevent or minimize the progression of diabetic neuropathy.
Symptoms and Complications of Diabetic Neuropathy
The symptoms of diabetic neuropathy can vary from person to person, but common signs include:
- numbness,
- tingling, and
- burning sensations in the hands and feet.
Some individuals may experience sharp or shooting pain, while others may have difficulty feeling hot or cold temperatures.
Dr. K. P. V. Rao’s Health Blogs
Diabetic neuropathy can also lead to
- muscle weakness,
- balance problems, and
- difficulty walking.
If left untreated, it can result in severe complications such as
- diabetic foot ulcers,
- infections, and
- even lead to amputations of the foot.
Diagnosing Diabetic Neuropathy
Apart from regular tests for diabetes like blood sugar levels and HbA1C, your doctor wll be carrying some specific tests. This usually involves a comprehensive evaluation of a patient’s medical history, physical examination, and specific tests.
A healthcare provider will typically assess symptoms, perform a neurological examination, and order blood tests to measure blood sugar levels and check for other potential causes of nerve damage.
Nerve conduction studies and electromyography can provide additional information about nerve function and help confirm the diagnosis in diabetic neuropathy. You can learn more about these tests here-
Diabetic neuropathy (Doc) by K P Vasudeva RaoTypes of Diabetic Neuropathy
There are four main types of this condition:
- **Peripheral neuropathy**: The most common form of diabetic neuropathy. It affects the feet and legs first, followed by the hands and arms. Symptoms include
- numbness or reduced ability to feel pain or temperature changes,
- tingling or burning sensation,
- sharp pain that may be worse at night,
- extreme sensitivity to touch,
- muscle weakness,
- loss of reflex response, and
- serious foot problems such as ulcers, infections, deformities, and bone and joint damage.
- **Autonomic neuropathy**: This type affects the nerves that control your blood pressure, heart rate, sweat glands, eyes, bladder, digestive system and sex organs. Symptoms include
- a lack of awareness that blood sugar levels are low (hypoglycemia unawareness),
- bladder problems such as frequent urinary tract infections, loss of bladder control (urinary incontinence) or trouble emptying the bladder (urinary retention),
- constipation, uncontrolled diarrhea or a combination of the two, slow stomach emptying (gastroparesis) leading to nausea, vomiting, sensation of fullness and loss of appetite,
- difficulty swallowing,
- erectile dysfunction in men,
- vaginal dryness and other sexual difficulties in women,
- increased or decreased sweating,
- drops in blood pressure when rising from sitting or lying down that may cause feelings of lightheadedness or fainting (orthostatic hypotension),
- problems regulating your body temperature,
- changes in the way your eyes adjust from light to dark or distance to nearness and
- increased heart rate even when you’re at rest.
- **Proximal neuropathy (diabetic polyradiculopathy) **: This type affects nerves in the thighs, hips, buttocks or legs. It is more common in people who have type 2 diabetes and in older adults. Symptoms are same as that of peripheral neuropathy and are usually felt on one side of the body but may spread to the other side too.
- **Focal neuropathies**: “Focal” refers to a particular or a specific point in the body. This type affects any single nerve or group of nerves anywhere in the body at any time. Symptoms depend on which nerve is affected and include sudden weakness or pain in one nerve area.
It’s important to note that most types of diabetic neuropathy develop gradually, and you may not notice problems until considerable damage has occurred. If you experience any symptoms mentioned above or have any concerns about your health condition, please consult your healthcare provider.
Traditional Treatments for Diabetic Neuropathy
Traditionally, the management of diabetic neuropathy has focused on controlling blood sugar levels, relieving pain, and managing complications.
Medications such as antidepressants, anticonvulsants, and opioids have been commonly prescribed to help alleviate neuropathic pain.
Commonly used medicines to treat DN
There are several medications available to help manage the symptoms of diabetic neuropathy. The following are some of the most commonly used medications :
- Duloxetine (Cymbalta): This is the only tricyclic antidepressant that has been approved by the FDA for treating the pain associated with diabetic neuropathy. It works by increasing the levels of certain chemicals in the brain that help reduce pain signals .
- Pregabalin (Lyrica): This is an anticonvulsant and analgesic that has been approved by the FDA for diabetic neuropathy. It works by reducing the number of pain signals sent out by damaged nerves in the body .
- These medications- Duloxetine and Pregabalin– work by modulating neurotransmitter activity and reducing nerve hyperexcitability.
- Tapentadol [extended release] (Nucynta ER): This is a centrally acting analgesic that has been approved by the FDA for treating diabetic neuropathy pain. It works by binding to certain receptors in the brain and spinal cord to reduce pain signals . Tapentadol provides dual mechanisms of action by combining opioid receptor agonism and norepinephrine reuptake inhibition. It offers effective pain relief while minimizing the side effects commonly associated with traditional opioids.
It’s important to note that these medications may not work for everyone and may have side effects. You should always consult your healthcare provider before taking any medication.
It’s important to note that medication choices should be made in consultation with your doctor or neurologist, taking into consideration individual needs, potential side effects, and drug interactions. A personalized treatment approach is essential to ensure the best possible outcomes for each patient.
Dr. K. P. V. Rao’s Health Blogs
Physical therapy, occupational therapy, and lifestyle modifications have also been recommended to improve function and reduce symptoms.
While these treatments have provided some relief, the latest breakthroughs in managing diabetic neuropathy offer even more promising options.
Latest Breakthroughs in Managing Diabetic Neuropathy
Advancements in medical research and technology have paved the way for innovative therapies that target the underlying mechanisms of diabetic neuropathy.
One of the most exciting breakthroughs is nerve stimulation, specifically
- Spinal cord stimulation (SCS) and
- Peripheral nerve stimulation (PNS).
These techniques involve the use of implanted devices that deliver electrical pulses to the nerves, effectively blocking pain signals and providing long-term relief. Clinical studies have shown significant reductions in pain and improved quality of life in patients who have undergone nerve stimulation.
For more on these techniques, read here-
Diabetic neuropathy (Doc) by K P Vasudeva RaoAnother promising breakthrough is the use of stem cell therapy for diabetic neuropathy. Stem cells have the potential to regenerate damaged nerves and improve nerve function. Early studies have shown promising results, but more research is needed to determine the long-term effectiveness and safety of this therapy.
Additionally, researchers are exploring the use of gene therapy and neuroprotective agents to prevent or slow down the progression of diabetic neuropathy. For more on these novel therapies, read this-
Diabetic neuropathy (Doc) by K P Vasudeva RaoThese novel approaches aim to target the specific molecular pathways involved in nerve damage and promote nerve repair and regeneration.
Lifestyle Changes and Self-Care Tips for Managing Diabetic Neuropathy
While breakthrough therapies and medications offer significant relief, lifestyle changes and self-care practices play a crucial role in managing diabetic neuropathy.
Maintaining healthy blood sugar levels through proper diet, regular exercise, and medication adherence is essential in preventing further nerve damage.
Quitting smoking and managing other risk factors such as high blood pressure can also help slow down the progression of neuropathy.
Additionally, self-care practices such as daily foot inspections, proper foot care, and wearing appropriate footwear can reduce the risk of developing foot ulcers and infections.
Regular exercise, including low-impact activities like swimming and cycling, can improve circulation and promote nerve health.
Stress management techniques, such as meditation and deep breathing exercises, may also help reduce pain and improve overall well-being.
Complications of Untreated Diabetic Neuropathy
If left untreated, diabetic neuropathy can lead to severe complications that significantly impact a person’s quality of life. Some of the commonly seen complications are:
- Diabetic foot ulcers, which result from nerve damage and reduced blood flow to the feet, can become infected and may require amputation if not properly treated.
- Charcot’s foot, a condition in which the bones in the foot weaken and fracture, and
- Autonomic neuropathy, which affects the nerves that control bodily functions such as digestion, heart rate, and blood pressure. Recognizing the importance of early intervention and effective management is crucial in preventing these complications.
Conclusion: Living Well with Diabetic Neuropathy
Living with diabetic neuropathy doesn’t have to be a constant struggle. With the latest breakthroughs in managing the condition and the availability of effective medications, relief and hope are within reach.
By staying informed about the latest advancements, individuals with diabetic neuropathy can work with their healthcare providers to develop a comprehensive treatment plan that addresses their specific needs.
Remember, managing diabetic neuropathy is a collaborative effort that requires a combination of medical interventions, lifestyle changes, and self-care practices. With the right approach, it is possible to live well and minimize the impact of diabetic neuropathy on daily life.
Final Words
I hope this article has proved useful to you. Kindly help me promote my articles by clicking on the social icons at the bottom of this artcle. If you have a X [formerly Twitter] account, do promote by clicking here-
Managing Diabetic Neuropathy: The Latest Breakthroughs and Medicines for Effective Relief Share on XStay tuned for other interesting articles like this by subscribing to my blogs.
Adios.