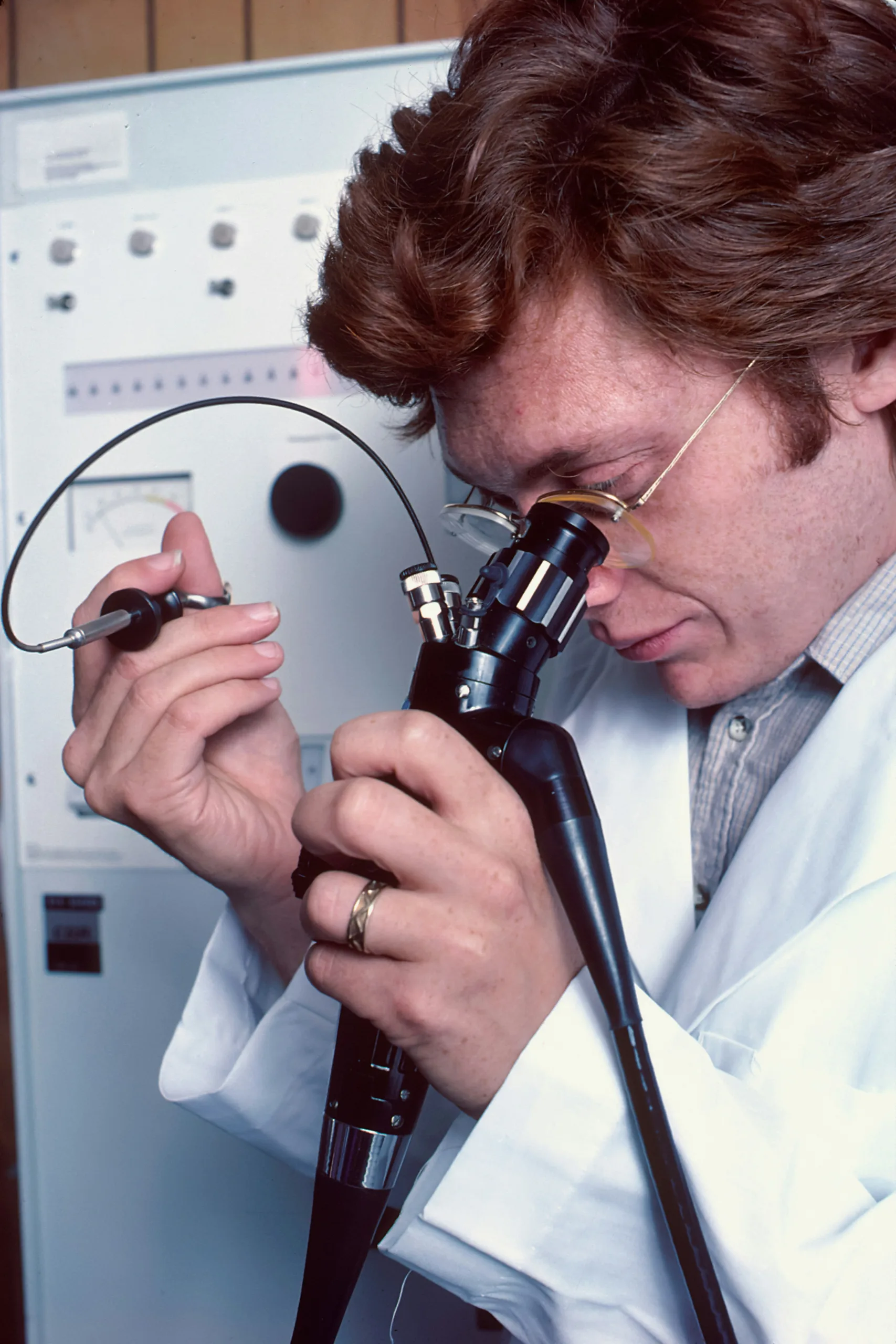
Understanding Bronchoscopy and Thoracoscopy: 2 valuable tools for Lower Respiratory Tract Diseases Diagnosis Exploring Diagnostic Procedures for Respiratory Conditions:- Listen...
Bronchoscopy and Thoracoscopy:2 Important tools to Diagnose LRTIBronchoscopy and Thoracoscopy:2 Important tools to Diagnose LRTI