MALARIA FEVER
Table of Contents
Introduction
Malaria fever is only next to Dengue and chikungunya spread by mosquitos. In this disease, a female anopheles’ mosquito [shown below] is a culprit. They feed in the night on human blood and breed during the daytime.

These mosquitoes transmit the malaria parasite from person to person by their bites.
Why I am writing this article?
As you all know, I am a General Medical practicing in Navi Mumbai, India. Every monsoon after a few days of heavy rains, water stagnates at many places serving as breeding places for Dengue and Malaria causing mosquitos. Many patients with fever attend my clinic. They are either suffering from Malaria or dengue.
Children and the elderly are more susceptible to a severe form of malaria. To make this aware to all my readers, I decided to write a comprehensive article describing everything you may want to know about the disease.
My motto has always been-Prevention is Better than Cure! That is the sole purpose of this a,rticle.
I request all my readers to read the article until the end to understand it fully. If possible, bookmark this on your browser so that you can refer to it anytime in the future.
What is Malaria and what causes it?
It is a form of fever that can make you very sick. Dengue fever discussed in my previous article[click here to read] was caused by a virus.
Malaria is caused by a protozoan parasite called Plasmodium and is transmitted/spread by the bite of mosquitos.
A Brief History of Malaria–
Many centuries ago, malaria existed in the gorillas in the African subcontinent. They were transmitted to human beings by Anopheles mosquitoes.

From Africa, the disease spread all over the world and is still causing havoc in South America, India, China, and other countries. This picture map shows how Malaria is ruling in different countries-
Transmission of Malaria parasite – The Pathophysiology of Malaria-
One should know how one gets Malaria. The picture shown below shows how exactly the malarial parasite is transmitted and spread by the female anopheles mosquito.

As the parasite enters the human body, it undergoes various stages. This goes on until it is picked up again by another mosquito. So, less or no exposure to mosquito bites should be your first concern.
Types of Species of Malaria parasites-
There are 4 types of malaria parasites-called Plasmodium[P.]– depending on which part of the world they are found-
1. Plasmodium Falciparum-
Found almost all over the world. This the most dangerous of the four varieties. India is also a host to this parasite. It can cause a severe form of malaria affecting the brain[Cerebral Malaria] and the kidney[Black water fever].
Fever occurs every day with rigors[shivering] and can reach up to 107° Fahrenheit.
2. P.Vivax –
This is also found worldwide, is less dangerous but can cause severe illness. Found in India. The disease caused by this variety is milder but can sometimes mimic P.Falciparum.
Fever can occur on alternate days or every 4th day.
3.Plasmodium Ovale-
Such type of malaria is found in Latin America and many Southeast Asian countries including India[rare]. This has a very low presence and is not that dangerous.
4.P.Malariae-
Found mostly in the Far East countries like Malaysia, Thailand, Vietnam. and China. Incidence is the same as that of P.Ovale.
Useful resource : https://www.cdc.gov/malaria/hcp/clinical-guidance/index.html
Signs and symptoms of Malaria-
All the symptoms are related to the phases of the development of the malarial parasite in the body and circulating blood[see the pathophysiology picture above]. The fever usually occurs in the schizont and merozoite stage, that is when the parasite enters the bloodstream from the liver[merozoite stage] to enter the red blood cell.
Next is when it breaks from the RBCs [ schizont stage]
The major symptoms of this disease are-
A] Fever-
Pyrexia or fever can range anywhere from 100°F to 107°F. The fever is intermittent. Depending on the type of malaria they are further classified as follows-
- Tertian fever- This occurs every 48 hours in P.Falciparum, P.Vivax, and P.Ovale.
- Quartan Fever- this occurs in P.Malariae
- Malignant fever- This is a feature of severe P.Falciparum malaria. It can lead to multi-organ failure[more on this in complications] and ultimately death if not treated in time. These patients need to be admitted to an ICU unit.
B] Rigors or Shivering-
Just before the fever begins, the patient starts shivering vigorously with the chattering of teeth. This called rigor. This is also called the Cold Stage.
C] Severe headache and body ache–
Fever and shivering are followed by severe headache, body ache, and pain in the eyes.
D] Vomiting, diarrhea, cough-
A few patients have severe bouts of vomiting and some, diarrhea [Seen in Intestinal malaria- a rare occurrence]. This can lead to the patient getting dehydrated and lethargic.
E] The Signs–
As the disease progresses, there is an enlargement of the liver and another organ called the spleen due to which there is a pain in these organs.
The liver gets enlarged because the parasites are multiplying there[ hepatic schizont stage].
Spleen is known as the graveyard of RBCs. After the release of the parasite from RBCs, the RBCs are scavenged by the spleen, enlarging it as the disease progresses.
F] Recovery phase-
The above symptoms last for a good 2-3 hours. After this, the recovery begins with the patient feeling very tired and wanting to sleep.
What are laboratory investigations for malaria?
Blood tests commonly recommended are
a] Complete blood checkup[CBC]- this will, in almost all cases, show-
- Anemia i.e. low hemoglobin levels
- Reduced RBC count
- Decreased Platelet count[ normal range 1.5 to 4.5 lakhs]
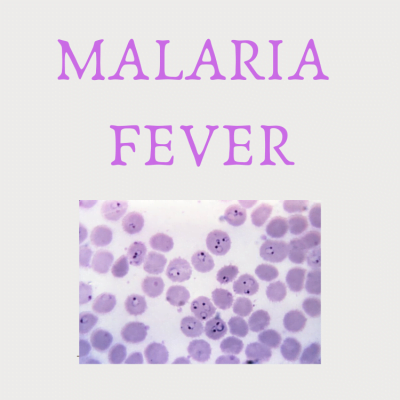
b] Smear for malaria parasite[MP] to confirm the diagnosis and show
- Type of malaria parasite
- The percentage of affected RBCs-more than 2% can lead to severe complications and death.
- Stage of development of the parasite, for eg., Schizont, or trophozoites or merozoite stage.
c] You can also have an immunological card test to confirm the type of malaria.
Having understood the Signs and symptoms, we now move to the treatment part.
Treatment Of Malaria:-
Drugs used commonly in the treatment are:-
- Chloroquine- This the most prescribed drug[ eg. Lariago, Nivaquin]. This is a 3-day course.
- Primaquine-Given after Choroquine dose is over. Should be taken for 14 consecutive days. I usually prescribe folic acid tablets[Folvite] with primaquine, as there is always acute folate deficiency in malaria.
- Mefloquine-rarely given nowadays;
- Quinine-Dosage depends upon body weight.
- Artesunate-Given in severe malaria. The dosage depends upon the severity of malaria.
- Artemether- Same as Artesunate
etc. to name a few.
Let your family physician decide the dosage and the type of medicine to be prescribed to you.
Kindly do not attempt to self-treat yourself as these medicines have severe side-effects. Better to leave it to your Family physician to take care of you.
Along with the antimalarial drugs you will also be prescribed-
- Paracetamol[ Crocin, Calpol, Pacimol] for fever;
- Domperidone[Domstal DT, Domperon] for nausea and vomiting;
- Chlorpheneramine[Avil] to prevent shivering and itching:
- Diclofenac/Ibuprofen[ Voveron, Diclogem, Ibugesic].
- Intravenous[IV] fluids if patients are vomiting continuously, with 5% glucose or ringer lactate. This can prevent severe dehydration.
A word of Caution-
If you have G-6PD deficiency or anyone in your family has this, kindly let your doctor know about it. This can prevent severe complications of malaria treatment.
G-6PD deficiency causes a condition called Hemolysis, wherein the RBCs in the blood are destroyed. Some antimalarials, especially Chloroquine and Primaquine, can cause severe hemolysis leading to jaundice and death in G-6PD deficient patients.
Non-medical treatment-
This consists of-
- Plenty of fluids, preferably with glucose or some powder like Vital-Z, Enerzal;
- Proper diet;
- Fruits
- Adequate bed-rest until full recovery. Avoid doing any form of exercise during the treatment period.
Complications of malaria-
Two types —P.vivax, and P.falciparum— are very common in India. Out of these two, P.vivax is less dangerous than P.falciparum.
The later one can cause multi-organ failures like-
- Kidney failure-wherein you may pass coffee-colored urine[so-called black-water fever],
- Brain fever -also called cerebral malaria, where the patient can go into a coma
- Blindness -due to choking of eye blood vessels, etc.
These patients need urgent admission in the hospital because they are very sick and need intravenous fluids like glucose-saline etc. and also to prevent complications of malaria, like coma, dehydration, congestive cardiac failure, etc.
Is there any immunity to the disease?
There is a small group of people having what we call the Sickle Cell Trait who are immune to malaria. People with Sickle cell trait are found immune to malaria. The reason is the parasite requires a lot of oxygen to survive. This is less in Sickle cell trait as the RBCs of these people are deformed i.e. shaped like a sickle.
These traits are found in tribals and poor people who lack money to get treated. These people over the years develop natural immunity in the form of deformed RBCs from trying to fight the disease.
Can you Prevent Malaria?
Yes, definitely. I would like to add a few words on the prevention of malaria because prevention is far better than cure. Kindly follow the following steps:-
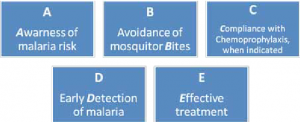
I preferably advise chemoprophylaxis if at least one member from the family has suffered from malaria.
What is Chemoprophylaxis? Is there a vaccine?
So far, no vaccine has been found for preventing malaria. Therefore, prevention or prophylaxis with drugs is the only way out.
Chemoprophylaxis is basically a medicine given to prevent disease. In Malaria, chloroquine is prescribed 2 tablets a week to all the family members who had a member suffering from the disease.
Other than that, a tablet combination of Pyrimethamine and Sulfadoxin[Reziz] is given on a monthly basis.
Some personal observations which can be useful to all-
- Use full-sleeved hosiery material shirts and pants-the the mosquitos find it difficult to pierce through these types of clothes.
- Never wear dark or black colored clothes-it camouflages the mosquitos[you can see them hiding in dark places or on furniture that is dark-colored].
- If you see a large mosquito parking on the ceiling, it is mostly a female anopheles one. Aedes Aegypti mosquitoes are small and will hide under furniture.
What else should you do to prevent malaria?
I personally use mosquito repellents such as mosquito repellent coils, patches, fabric roll-ons, window nets etc. These are easily available online.
To know more about malaria, you can click here.
What can you as readers do to make the world a better place to live in-
Friends, as you all know the whole world is up against the Covid-19 pandemic. During this period, Malaria can overlap with the COVID-19 pandemic.
There is a saying “Sharing is Caring”. I have done my bit by getting this article to you. Now, you can contribute, without spending a penny by sharing this information with all those you love and care for.
Do this now by clicking on the Social Media icons in this article with a small note” Read this article”.
Alternately, if you have a Twitter account, you can just click on the quote below-
Stay Informed, Stay Healthy- Let us together Fight Covid-19 and Malaria Share on XAs usual, I would like to add-if you have any queries, you can leave a message in the comments section. I will be glad to help and guide you.